CIC Exam Question 11
Following recent renovations on an oncology unit, three patients were identified with Aspergillus infections.
The infections were thought to be facility-acquired. Appropriate environmental microbiological monitoring would be to culture the:
The infections were thought to be facility-acquired. Appropriate environmental microbiological monitoring would be to culture the:
Correct Answer: A
The scenario describes an outbreak of Aspergillus infections among three patients on an oncology unit following recent renovations, with the infections suspected to be facility-acquired. Aspergillus is a mold commonly associated with environmental sources, particularly airborne spores, and its presence in immunocompromised patients (e.g., oncology patients) poses a significant risk. The infection preventionist must identify the appropriate environmental microbiological monitoring strategy, guided by the Certification Board of Infection Control and Epidemiology (CBIC) and CDC recommendations. Let's evaluate each option:
* A. Air: Aspergillus species are ubiquitous molds that thrive in soil, decaying vegetation, and construction dust, and they are primarily transmitted via airborne spores. Renovations can disturb these spores, leading to aerosolization and inhalation by vulnerable patients. Culturing the air using methods such as settle plates, air samplers, or high-efficiency particulate air (HEPA) filtration monitoring is a standard practice to detect Aspergillusduring construction or post-renovation in healthcare settings, especially oncology units where patients are at high risk for invasive aspergillosis. This aligns with CBIC's emphasis on environmental monitoring for airborne pathogens, making it the most appropriate choice.
* B. Ice: Ice can be a source of contamination with bacteria (e.g., Pseudomonas, Legionella) or other pathogens if improperly handled or stored, but it is not a typical reservoir for Aspergillus, which is a mold requiring organic material and moisture for growth. While ice safety is important in infection control, culturing ice is irrelevant to an Aspergillus outbreak linked to renovations and is not a priority in this context.
* C. Carpet: Carpets can harbor dust, mold, and other microorganisms, especially in high-traffic or poorly maintained areas. Aspergillus spores could theoretically settle in carpet during renovations, but carpets are not a primary source of airborne transmission unless disturbed (e.g., vacuuming). Culturing carpet might be a secondary step if air sampling indicates widespread contamination, but it is less direct and less commonly recommended as the initial monitoring site compared to air sampling.
* D. Aerators: Aerators (e.g., faucet aerators) can harbor waterborne pathogens like Pseudomonas or Legionella due to biofilm formation, but Aspergillus is not typically associated with water systems unless there is significant organic contamination or aerosolization from water sources (e.g., cooling towers). Culturing aerators is relevant for waterborne outbreaks, not for an Aspergillus outbreak linked to renovations, making this option inappropriate.
The best answer is A, culturing the air, as Aspergillus is an airborne pathogen, and renovations are a known risk factor for spore dispersal in healthcare settings. This monitoring strategy allows the infection preventionist to confirm the source, assess the extent of contamination, and implement control measures (e.g., enhanced filtration, construction barriers) to protect patients. This is consistent with CBIC and CDC guidelines for managing fungal outbreaks in high-risk units.
:
CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain IV:
Environment of Care, which recommends air sampling for Aspergillus during construction-related outbreaks.
CBIC Examination Content Outline, Domain III: Prevention and Control of Infectious Diseases, which includes environmental monitoring for facility-acquired infections.
CDC Guidelines for Environmental Infection Control in Healthcare Facilities (2022), which advocate air culturing to detect Aspergillus post-renovation in immunocompromised patient areas.
* A. Air: Aspergillus species are ubiquitous molds that thrive in soil, decaying vegetation, and construction dust, and they are primarily transmitted via airborne spores. Renovations can disturb these spores, leading to aerosolization and inhalation by vulnerable patients. Culturing the air using methods such as settle plates, air samplers, or high-efficiency particulate air (HEPA) filtration monitoring is a standard practice to detect Aspergillusduring construction or post-renovation in healthcare settings, especially oncology units where patients are at high risk for invasive aspergillosis. This aligns with CBIC's emphasis on environmental monitoring for airborne pathogens, making it the most appropriate choice.
* B. Ice: Ice can be a source of contamination with bacteria (e.g., Pseudomonas, Legionella) or other pathogens if improperly handled or stored, but it is not a typical reservoir for Aspergillus, which is a mold requiring organic material and moisture for growth. While ice safety is important in infection control, culturing ice is irrelevant to an Aspergillus outbreak linked to renovations and is not a priority in this context.
* C. Carpet: Carpets can harbor dust, mold, and other microorganisms, especially in high-traffic or poorly maintained areas. Aspergillus spores could theoretically settle in carpet during renovations, but carpets are not a primary source of airborne transmission unless disturbed (e.g., vacuuming). Culturing carpet might be a secondary step if air sampling indicates widespread contamination, but it is less direct and less commonly recommended as the initial monitoring site compared to air sampling.
* D. Aerators: Aerators (e.g., faucet aerators) can harbor waterborne pathogens like Pseudomonas or Legionella due to biofilm formation, but Aspergillus is not typically associated with water systems unless there is significant organic contamination or aerosolization from water sources (e.g., cooling towers). Culturing aerators is relevant for waterborne outbreaks, not for an Aspergillus outbreak linked to renovations, making this option inappropriate.
The best answer is A, culturing the air, as Aspergillus is an airborne pathogen, and renovations are a known risk factor for spore dispersal in healthcare settings. This monitoring strategy allows the infection preventionist to confirm the source, assess the extent of contamination, and implement control measures (e.g., enhanced filtration, construction barriers) to protect patients. This is consistent with CBIC and CDC guidelines for managing fungal outbreaks in high-risk units.
:
CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain IV:
Environment of Care, which recommends air sampling for Aspergillus during construction-related outbreaks.
CBIC Examination Content Outline, Domain III: Prevention and Control of Infectious Diseases, which includes environmental monitoring for facility-acquired infections.
CDC Guidelines for Environmental Infection Control in Healthcare Facilities (2022), which advocate air culturing to detect Aspergillus post-renovation in immunocompromised patient areas.
CIC Exam Question 12
When assessing a patient's infection prevention and control educational needs, it is necessary to FIRST determine the patient's
Correct Answer: D
The correct answer is D, "baseline knowledge of the subject," as this is the necessary first step when assessing a patient's infection prevention and control educational needs. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, effective patient education in infection prevention and control requires a tailored approach that begins with understanding the patient's existing knowledge and comprehension of the topic. Determining baseline knowledge allows the infection preventionist (IP) to identify gaps, customize educational content to the patient's level of understanding, and ensure the information is relevant and actionable (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.1 - Develop and implement educational programs). This step ensures that education is neither too basic nor overly complex, maximizing its effectiveness in promoting behaviors such as hand hygiene, wound care, or adherence to isolation protocols.
Option A (severity of illness) is an important clinical consideration that may influence the timing or method of education delivery, but it is not the first step in assessing educational needs. The severity might affect the patient's ability to learn, but it does not directly inform the content or starting point of the education. Option B (educational background) provides context about the patient's general learning capacity (e.g., literacy level or language preference), but it is secondary to assessing specific knowledge about infection prevention, as background alone does not reveal current understanding. Option C (duration of hospitalization) may impact the opportunity for education but is not a primary factor in determining what the patient needs to learn; it is more relevant to scheduling or prioritizing educational interventions.
The focus on baseline knowledge aligns with adult learning principles endorsed by CBIC, which emphasize assessing learners' prior knowledge to build effective educational strategies (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs).
This approach ensures patient-centered care and supports infection control by empowering patients with the knowledge to participate in their own prevention efforts.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.1 - Develop and implement educational programs, 4.2 - Evaluate the effectiveness of educational programs.
Option A (severity of illness) is an important clinical consideration that may influence the timing or method of education delivery, but it is not the first step in assessing educational needs. The severity might affect the patient's ability to learn, but it does not directly inform the content or starting point of the education. Option B (educational background) provides context about the patient's general learning capacity (e.g., literacy level or language preference), but it is secondary to assessing specific knowledge about infection prevention, as background alone does not reveal current understanding. Option C (duration of hospitalization) may impact the opportunity for education but is not a primary factor in determining what the patient needs to learn; it is more relevant to scheduling or prioritizing educational interventions.
The focus on baseline knowledge aligns with adult learning principles endorsed by CBIC, which emphasize assessing learners' prior knowledge to build effective educational strategies (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs).
This approach ensures patient-centered care and supports infection control by empowering patients with the knowledge to participate in their own prevention efforts.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.1 - Develop and implement educational programs, 4.2 - Evaluate the effectiveness of educational programs.
CIC Exam Question 13
Therapeutic antimicrobial agents should be used when
Correct Answer: D
Therapeutic antimicrobial agentsshould ideally bepathogen-directedto minimizeresistance, side effects, and treatment failure. Once thecausative pathogen and its antimicrobial susceptibilities are known, the mostnarrow-spectrum, effectiveagent should be used.
Why the Other Options Are Incorrect?
* A. The infecting agent is unknown- Empiric therapy may be necessary initially, but definitive therapy should be based on pathogen identification.
* B. The patient's illness warrants treatment prior to culture results- This applies toempiric therapy
, but not todefinitive antimicrobial selection.
* C. The patient's symptoms suggest likely pathogens- Clinical presentation guidesempiric treatment
, butdefinitive therapy should follow culture and susceptibility testing.
CBIC Infection Control Reference
APIC emphasizes theimportance of selecting antimicrobials based on pathogen identification and susceptibility testingto preventantimicrobial resistance.
Why the Other Options Are Incorrect?
* A. The infecting agent is unknown- Empiric therapy may be necessary initially, but definitive therapy should be based on pathogen identification.
* B. The patient's illness warrants treatment prior to culture results- This applies toempiric therapy
, but not todefinitive antimicrobial selection.
* C. The patient's symptoms suggest likely pathogens- Clinical presentation guidesempiric treatment
, butdefinitive therapy should follow culture and susceptibility testing.
CBIC Infection Control Reference
APIC emphasizes theimportance of selecting antimicrobials based on pathogen identification and susceptibility testingto preventantimicrobial resistance.
CIC Exam Question 14
Surgical site infection (SSI) data for the previous quarter reveal the following numbers. The surgeon with the highest infection rate is Doctor


Correct Answer: D
To determine which surgeon has the highest surgical site infection (SSI) rate, use the following formula:
A screenshot of a report AI-generated content may be incorrect.
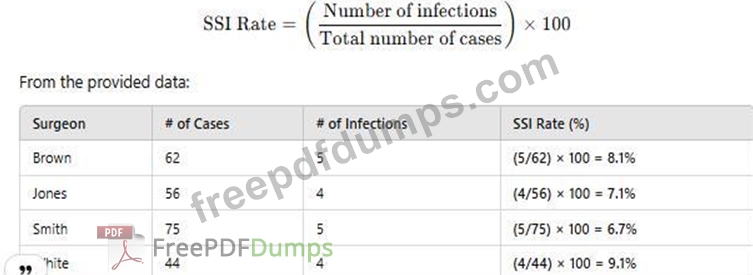
Since Dr. White has the highest SSI rate at 9.1%, the correct answer is D. White.
CBIC Infection Control Reference
SSI rates are calculated using infection count per total procedures and reported as percentage values.
A screenshot of a report AI-generated content may be incorrect.
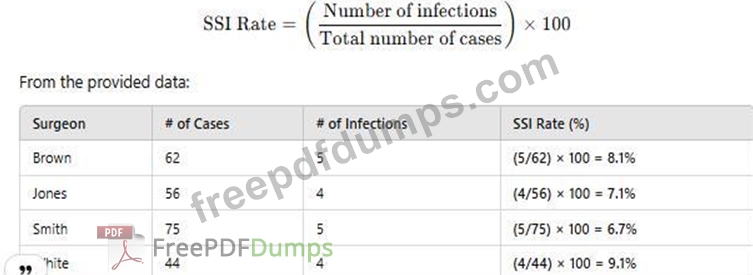
Since Dr. White has the highest SSI rate at 9.1%, the correct answer is D. White.
CBIC Infection Control Reference
SSI rates are calculated using infection count per total procedures and reported as percentage values.
CIC Exam Question 15
Essential knowledge, behaviors, and skills that an individual should possess and demonstrate to practice in a specific discipline defines which of the following?
Correct Answer: B
The correct answer is B, "Competence," as it defines the essential knowledge, behaviors, and skills that an individual should possess and demonstrate to practice in a specific discipline. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, competence encompasses the integrated application of knowledge, skills, and behaviors required to perform effectively in a professional role, such as infection prevention and control. Competence goes beyond mere knowledge or training by including the ability to apply these attributes in real-world scenarios, ensuring safe and effective practice (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.3 - Assess competence of healthcare personnel). This holistic definition is critical in healthcare settings, where demonstrated competence-through actions like proper hand hygiene or outbreak management-directly impacts patient safety and infection prevention outcomes.
Option A (certification) refers to a formal recognition or credential (e.g., CIC certification) that validates an individual's qualifications, but it is an outcome or process rather than the definition of the underlying abilities.
Option C (knowledge) represents the theoretical understanding or factual basis of a discipline, which is a component of competence but not the full scope that includes behaviors and skills. Option D (training) involves the education or instruction provided to develop skills and knowledge, serving as a means to achieve competence rather than defining it.
The focus on competence aligns with CBIC's emphasis on ensuring that healthcare personnel are equipped to meet the demands of infection prevention through a combination of education, practice, and evaluation (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This definition supports the development of professionals who can adapt and perform effectively in dynamic healthcare environments.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.2 - Evaluate the effectiveness of educational programs, 4.3 - Assess competence of healthcare personnel.
Option A (certification) refers to a formal recognition or credential (e.g., CIC certification) that validates an individual's qualifications, but it is an outcome or process rather than the definition of the underlying abilities.
Option C (knowledge) represents the theoretical understanding or factual basis of a discipline, which is a component of competence but not the full scope that includes behaviors and skills. Option D (training) involves the education or instruction provided to develop skills and knowledge, serving as a means to achieve competence rather than defining it.
The focus on competence aligns with CBIC's emphasis on ensuring that healthcare personnel are equipped to meet the demands of infection prevention through a combination of education, practice, and evaluation (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This definition supports the development of professionals who can adapt and perform effectively in dynamic healthcare environments.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.2 - Evaluate the effectiveness of educational programs, 4.3 - Assess competence of healthcare personnel.
- Latest Upload
- 120SAP.C_THR89_2505.v2025-12-16.q58
- 133Huawei.H12-821_V1.0.v2025-12-16.q153
- 111Juniper.JN0-750.v2025-12-16.q35
- 159Microsoft.SC-200.v2025-12-15.q150
- 130Fortinet.FCSS_EFW_AD-7.6.v2025-12-15.q26
- 141Microsoft.SC-300.v2025-12-15.q140
- 150Microsoft.MS-900.v2025-12-15.q191
- 137Avaya.78202T.v2025-12-14.q94
- 149EMC.D-PST-DY-23.v2025-12-14.q89
- 122HP.HPE0-S59.v2025-12-14.q35

