CIC Exam Question 71
Healthcare workers are MOST likely to benefit from infection prevention education if the Infection Preventionist (IP)
Correct Answer: D
The correct answer is D, "involves the staff in determining the content," as this approach is most likely to benefit healthcare workers from infection prevention education. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, effective education programs are tailored to the specific needs and contexts of the learners. Involving staff in determining the content ensures that the educational material addresses their real-world challenges, knowledge gaps, and interests, thereby increasing engagement, relevance, and application of the learned principles (CBIC Practice Analysis, 2022, Domain IV:
Education and Research, Competency 4.1 - Develop and implement educational programs). This participatory approach fosters ownership and accountability among healthcare workers, enhancing the likelihood that they will adopt and sustain infection prevention practices.
Option A (brings in speakers who are recognized experts) can enhance credibility and provide high-quality information, but it does not guarantee that the content will meet the specific needs of the staff unless their input is considered. Option B (plans the educational program well ahead of time) is important for logistical success and preparedness, but without staff involvement, the program may lack relevance or fail to address immediate concerns. Option C (audits practices and identifies deficiencies) is a valuable step in identifying areas for improvement, but it is a diagnostic process rather than a direct educational strategy; education based solely on audits might not engage staff effectively if their input is not sought.
The focus on involving staff aligns with CBIC's emphasis on adult learning principles, which highlight the importance of learner-centered education. By involving staff, the IP adheres to best practices for adult education, ensuring that the program is practical and tailored, ultimately leading to better outcomes in infection prevention (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This approach also supports a collaborative culture, which is critical for sustaining infection control efforts in healthcare settings.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.1 - Develop and implement educational programs, 4.2 - Evaluate the effectiveness of educational programs.
Education and Research, Competency 4.1 - Develop and implement educational programs). This participatory approach fosters ownership and accountability among healthcare workers, enhancing the likelihood that they will adopt and sustain infection prevention practices.
Option A (brings in speakers who are recognized experts) can enhance credibility and provide high-quality information, but it does not guarantee that the content will meet the specific needs of the staff unless their input is considered. Option B (plans the educational program well ahead of time) is important for logistical success and preparedness, but without staff involvement, the program may lack relevance or fail to address immediate concerns. Option C (audits practices and identifies deficiencies) is a valuable step in identifying areas for improvement, but it is a diagnostic process rather than a direct educational strategy; education based solely on audits might not engage staff effectively if their input is not sought.
The focus on involving staff aligns with CBIC's emphasis on adult learning principles, which highlight the importance of learner-centered education. By involving staff, the IP adheres to best practices for adult education, ensuring that the program is practical and tailored, ultimately leading to better outcomes in infection prevention (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This approach also supports a collaborative culture, which is critical for sustaining infection control efforts in healthcare settings.
References: CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competencies 4.1 - Develop and implement educational programs, 4.2 - Evaluate the effectiveness of educational programs.
CIC Exam Question 72
Which of the following pathogens is associated with the highest risk of seroconversion after percutaneous exposure?
Correct Answer: D
Among the listed pathogens,Hepatitis Chas thehighest risk of seroconversion following a percutaneous exposure, though it's important to note thatHepatitis Bactually has the highest overall risk. However, since Hepatitis B is not listed among the options, the correct choice from the available ones isHepatitis C.
* TheAPIC Textconfirms:
"The average risk of seroconversion after a percutaneous injury involving blood infected with hepatitis C virus is approximately 1.8 percent".
* The other options are not bloodborne pathogens typically associated with high seroconversion risks after needlestick or percutaneous exposure:
* A. Shigella- transmitted fecal-orally, not percutaneously.
* B. Syphilis- transmitted sexually or via mucous membranes.
* C. Hepatitis A- primarily fecal-oral transmission, low occupational seroconversion risk.
References:
APIC Text, 4th Edition, Chapter 103 - Occupational Exposure to Bloodborne Pathogens
* TheAPIC Textconfirms:
"The average risk of seroconversion after a percutaneous injury involving blood infected with hepatitis C virus is approximately 1.8 percent".
* The other options are not bloodborne pathogens typically associated with high seroconversion risks after needlestick or percutaneous exposure:
* A. Shigella- transmitted fecal-orally, not percutaneously.
* B. Syphilis- transmitted sexually or via mucous membranes.
* C. Hepatitis A- primarily fecal-oral transmission, low occupational seroconversion risk.
References:
APIC Text, 4th Edition, Chapter 103 - Occupational Exposure to Bloodborne Pathogens
CIC Exam Question 73
What rate is expressed by the number of patients who acquire infections over a specified time period divided by the population at risk of acquiring an infection during that time period?
Correct Answer: A
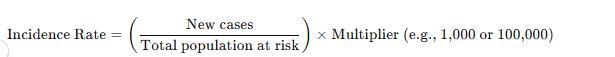
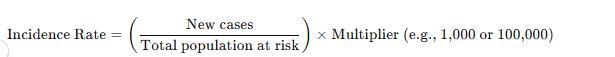
The incidence rate measures new cases of infection in a population over a defined time period using the formula:
Why the Other Options Are Incorrect?
* B. Disease specific - Refers to infections caused by a particular pathogen, not the general rate of new infections.
* C. Point prevalence - Measures existing cases at a specific point in time, not new cases.
* D. Period prevalence - Includes both old and new cases over a set period, unlike incidence, which only considers new cases.
CBIC Infection Control Reference
APIC defines incidence rate as the number of new infections in a population over a given period.
Why the Other Options Are Incorrect?
* B. Disease specific - Refers to infections caused by a particular pathogen, not the general rate of new infections.
* C. Point prevalence - Measures existing cases at a specific point in time, not new cases.
* D. Period prevalence - Includes both old and new cases over a set period, unlike incidence, which only considers new cases.
CBIC Infection Control Reference
APIC defines incidence rate as the number of new infections in a population over a given period.
CIC Exam Question 74
A 36-year-old female presents to the Emergency Department with a petechial rash, meningitis, and cardiac arrest. During the resuscitation, a phlebotomist sustained a needlestick injury. The next day, blood cultures reveal Neisseria meningitidis. The exposure management for the phlebotomist is:
Correct Answer: C
The scenario involves a needlestick injury sustained by a phlebotomist during the resuscitation of a patient diagnosed with Neisseria meningitidis infection, characterized by a petechial rash, meningitis, and cardiac arrest. Neisseria meningitidis is a gram-negative diplococcus that can cause meningococcal disease, including meningitis and septicemia, and is transmitted through direct contact with respiratory secretions or, in rare cases, blood exposure. The exposure management for the phlebotomist must align with infection control guidelines, such as those from the Certification Board of Infection Control and Epidemiology (CBIC) and the CDC, to prevent potential infection. Let's evaluate each option:
* A. Prophylactic rifampin plus isoniazid: Prophylactic antibiotics are recommended for close contacts of individuals with meningococcal disease to prevent secondary cases. Rifampin is a standard prophylactic agent for Neisseria meningitidis exposure, typically administered as a 2-day course (e.g., 600 mg every
12 hours for adults). Isoniazid, however, is used for tuberculosis (TB) prophylaxis and is not indicated for meningococcal disease. Combining rifampin with isoniazid is incorrect, as it reflects a confusion with TB management rather than meningococcal exposure. This option is not appropriate.
* B. A tuberculin skin test now and in ten weeks: A tuberculin skin test (TST) or interferon-gamma release assay (IGRA) is used to screen for latent tuberculosis infection, with a follow-up test at 8-10 weeks to detect conversion after potential TB exposure. Neisseria meningitidis is not related to TB, and a needlestick injury from a meningococcal patient does not warrant TB testing. This option is irrelevant to the scenario and not the correct exposure management.
* C. Work furlough from day ten to day 21 after exposure: Neisseria meningitidis has an incubation period of 2-10 days, with a maximum of about 14 days in rare cases. The CDC and WHO recommend that healthcare workers exposed to meningococcal disease via needlestick or mucosal exposure be monitored for signs of infection (e.g., fever, rash) and, if symptomatic, isolated and treated.
Additionally, a work restriction or furlough from day 10 to day 21 after exposure is advised to cover the potential incubation period, especially if prophylaxis is declined or contraindicated. This allows time to observe for symptoms and prevents transmission to vulnerable patients. This is a standard infection control measure and the most appropriate initial management step pending prophylaxis decision.
* D. A review of the phlebotomist's hepatitis B vaccine status: Reviewing hepatitis B vaccine status is a critical step following a needlestick injury, as hepatitis B can be transmitted through blood exposure.
However, this applies to bloodborne pathogens (e.g., HBV, HCV, HIV) and is not specific to Neisseria meningitidis, which is primarily a respiratory or mucosal pathogen. While hepatitis B management (e.
g., post-exposure prophylaxis with hepatitis B immunoglobulin or vaccine booster) should be addressed as part of a comprehensive needlestick protocol, it is not the first or most relevant priority for meningococcal exposure.
The best answer is C, as the work furlough from day 10 to day 21 after exposure addresses the specific risk of meningococcal disease following a needlestick injury. This aligns with CBIC's focus on timely intervention and work restriction to prevent transmission in healthcare settings. Prophylactic antibiotics (e.g., rifampin) should also be considered, but the question asks for the exposure management, and furlough is a primary control measure. Hepatitis B and TB considerations are secondary and managed separately.
References:
* CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain III:
Prevention and Control of Infectious Diseases, which includes protocols for managing exposure to communicable diseases like meningococcal infection.
* CBIC Examination Content Outline, Domain IV: Environment of Care, which addresses work restrictions and exposure management.
* CDC Guidelines for Meningococcal Disease Prevention and Control (2023), which recommend work furlough and monitoring for exposed healthcare workers.
* A. Prophylactic rifampin plus isoniazid: Prophylactic antibiotics are recommended for close contacts of individuals with meningococcal disease to prevent secondary cases. Rifampin is a standard prophylactic agent for Neisseria meningitidis exposure, typically administered as a 2-day course (e.g., 600 mg every
12 hours for adults). Isoniazid, however, is used for tuberculosis (TB) prophylaxis and is not indicated for meningococcal disease. Combining rifampin with isoniazid is incorrect, as it reflects a confusion with TB management rather than meningococcal exposure. This option is not appropriate.
* B. A tuberculin skin test now and in ten weeks: A tuberculin skin test (TST) or interferon-gamma release assay (IGRA) is used to screen for latent tuberculosis infection, with a follow-up test at 8-10 weeks to detect conversion after potential TB exposure. Neisseria meningitidis is not related to TB, and a needlestick injury from a meningococcal patient does not warrant TB testing. This option is irrelevant to the scenario and not the correct exposure management.
* C. Work furlough from day ten to day 21 after exposure: Neisseria meningitidis has an incubation period of 2-10 days, with a maximum of about 14 days in rare cases. The CDC and WHO recommend that healthcare workers exposed to meningococcal disease via needlestick or mucosal exposure be monitored for signs of infection (e.g., fever, rash) and, if symptomatic, isolated and treated.
Additionally, a work restriction or furlough from day 10 to day 21 after exposure is advised to cover the potential incubation period, especially if prophylaxis is declined or contraindicated. This allows time to observe for symptoms and prevents transmission to vulnerable patients. This is a standard infection control measure and the most appropriate initial management step pending prophylaxis decision.
* D. A review of the phlebotomist's hepatitis B vaccine status: Reviewing hepatitis B vaccine status is a critical step following a needlestick injury, as hepatitis B can be transmitted through blood exposure.
However, this applies to bloodborne pathogens (e.g., HBV, HCV, HIV) and is not specific to Neisseria meningitidis, which is primarily a respiratory or mucosal pathogen. While hepatitis B management (e.
g., post-exposure prophylaxis with hepatitis B immunoglobulin or vaccine booster) should be addressed as part of a comprehensive needlestick protocol, it is not the first or most relevant priority for meningococcal exposure.
The best answer is C, as the work furlough from day 10 to day 21 after exposure addresses the specific risk of meningococcal disease following a needlestick injury. This aligns with CBIC's focus on timely intervention and work restriction to prevent transmission in healthcare settings. Prophylactic antibiotics (e.g., rifampin) should also be considered, but the question asks for the exposure management, and furlough is a primary control measure. Hepatitis B and TB considerations are secondary and managed separately.
References:
* CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain III:
Prevention and Control of Infectious Diseases, which includes protocols for managing exposure to communicable diseases like meningococcal infection.
* CBIC Examination Content Outline, Domain IV: Environment of Care, which addresses work restrictions and exposure management.
* CDC Guidelines for Meningococcal Disease Prevention and Control (2023), which recommend work furlough and monitoring for exposed healthcare workers.
CIC Exam Question 75
Some pathogens live in the body and can be cultured, but do NOT elicit any response from the body's defense mechanisms. This state is called:
Correct Answer: A
The interaction between pathogens and the human body can take various forms, each with distinct immunological and clinical implications. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes understanding these states within the "Identification of Infectious Disease Processes" domain to guide infection prevention strategies. The question describes a scenario where pathogens are present, can be cultured (indicating viable organisms), but do not trigger a response from the body's defense mechanisms, such as inflammation or immune activation. This requires identifying the appropriate microbiological state.
Option A, "Colonization," is the correct answer. Colonization occurs when microorganisms are present on or in the body (e.g., skin, mucous membranes, or gut) without causing harm or eliciting an immune response.
These pathogens can be cultured, as they are alive and replicating, but they exist in a commensal or symbiotic relationship with the host, not provoking symptoms or defense mechanisms. Examples include normal flora like Staphylococcus epidermidis on the skin or Streptococcus salivarius in the oral cavity. The Centers for Disease Control and Prevention (CDC) defines colonization as the presence of microbes without tissue invasion or damage, distinguishing it from infection (CDC, "Principles of Epidemiology in Public Health Practice," 3rd Edition, 2012).
Option B, "Infection," is incorrect because it involves the invasion and multiplication of pathogens in body tissues, leading to an immune response, such as inflammation, fever, or antibody production. This contrasts with the question's description of no defense mechanism response. Option C, "Latency," refers to a state where a pathogen (e.g., herpes simplex virus or Mycobacterium tuberculosis) remains dormant in the body after initial infection, capable of reactivation but not eliciting an active immune response during dormancy.
However, latency implies a prior infection with a latent phase, whereas the question suggests a current, non- responsive state without prior infection context. Option D, "Contamination," describes the unintended presence of pathogens on inanimate objects or surfaces (e.g., medical equipment), not within the body, and does not align with the scenario of living, culturable pathogens in a host.
The CBIC Practice Analysis (2022) and CDC guidelines highlight colonization as a key concept in infection control, particularly in settings like hospitals where colonized patients can serve as reservoirs for potential infections. The absence of an immune response, as specified, aligns with the definition of colonization, making Option A the most accurate answer.
References:
* CBIC Practice Analysis, 2022.
* CDC Principles of Epidemiology in Public Health Practice, 3rd Edition, 2012.
Option A, "Colonization," is the correct answer. Colonization occurs when microorganisms are present on or in the body (e.g., skin, mucous membranes, or gut) without causing harm or eliciting an immune response.
These pathogens can be cultured, as they are alive and replicating, but they exist in a commensal or symbiotic relationship with the host, not provoking symptoms or defense mechanisms. Examples include normal flora like Staphylococcus epidermidis on the skin or Streptococcus salivarius in the oral cavity. The Centers for Disease Control and Prevention (CDC) defines colonization as the presence of microbes without tissue invasion or damage, distinguishing it from infection (CDC, "Principles of Epidemiology in Public Health Practice," 3rd Edition, 2012).
Option B, "Infection," is incorrect because it involves the invasion and multiplication of pathogens in body tissues, leading to an immune response, such as inflammation, fever, or antibody production. This contrasts with the question's description of no defense mechanism response. Option C, "Latency," refers to a state where a pathogen (e.g., herpes simplex virus or Mycobacterium tuberculosis) remains dormant in the body after initial infection, capable of reactivation but not eliciting an active immune response during dormancy.
However, latency implies a prior infection with a latent phase, whereas the question suggests a current, non- responsive state without prior infection context. Option D, "Contamination," describes the unintended presence of pathogens on inanimate objects or surfaces (e.g., medical equipment), not within the body, and does not align with the scenario of living, culturable pathogens in a host.
The CBIC Practice Analysis (2022) and CDC guidelines highlight colonization as a key concept in infection control, particularly in settings like hospitals where colonized patients can serve as reservoirs for potential infections. The absence of an immune response, as specified, aligns with the definition of colonization, making Option A the most accurate answer.
References:
* CBIC Practice Analysis, 2022.
* CDC Principles of Epidemiology in Public Health Practice, 3rd Edition, 2012.
- Latest Upload
- 120SAP.C_THR89_2505.v2025-12-16.q58
- 134Huawei.H12-821_V1.0.v2025-12-16.q153
- 112Juniper.JN0-750.v2025-12-16.q35
- 159Microsoft.SC-200.v2025-12-15.q150
- 131Fortinet.FCSS_EFW_AD-7.6.v2025-12-15.q26
- 141Microsoft.SC-300.v2025-12-15.q140
- 150Microsoft.MS-900.v2025-12-15.q191
- 137Avaya.78202T.v2025-12-14.q94
- 149EMC.D-PST-DY-23.v2025-12-14.q89
- 122HP.HPE0-S59.v2025-12-14.q35

